Medical Insurance Verification
Instant Patient Eligibility Checks Across 950+ Payers
Get fast, accurate eligibility and benefits verification right inside Salesforce with access to 950+ payers including Medicare and Medicaid. Check coverage, confirm benefits, and receive real-time authorizations while keeping costs low and workflows simple.
Know a Patient’s Coverage Before You Even Start
It’s stressful guessing whether a patient is actually covered, and it slows everyone down. With instant checks built right into Salesforce, your team gets clear answers on eligibility, benefits, and out-of-pocket costs in seconds. Fewer surprises mean smoother visits and fewer billing headaches later.



-p-1080%201.png)
Check 950+ Payers Without Leaving Salesforce
No more jumping between portals or calling payer lines. You get direct access to Medicare, Medicaid, and hundreds of commercial payers right inside your workflow. Real-time details help your staff act quickly instead of wasting time chasing information.



-p-1080%201.png)
Handle Approvals and Referrals Faster Than Ever
Waiting on authorizations slows everything down for both patients and staff. This tool pulls requirements instantly and helps you secure authorizations quickly so care isn’t delayed. Your team can move forward with confidence instead of hoping everything gets approved later.



-p-1080%201.png)
Protect Patient Data While Boosting Compliance
Healthcare teams worry about privacy for good reason. This system keeps everything encrypted, logged, and stored in a HIPAA-secure environment so your compliance team can relax. You get speed without sacrificing safety.



-p-1080%201.png)
Keep Everything Organized and Accurate Automatically
You don’t have to manually track coverage changes or shuffle between systems. Everything updates directly in Salesforce so your records stay clean, correct, and easy to follow. This cuts down on admin work and makes billing decisions much simpler.



-p-1080%201.png)
The Results Healthcare Teams Notice Quickly

Better coverage checks up front catch missing details early, helping teams submit cleaner claims and avoid the back-and-forth that slows reimbursement.

Instant payer responses speed up patient intake, letting staff verify coverage and benefits without long calls or portal hopping during busy clinic hours.

Procedure-specific verification prevents unpaid services by confirming coverage before treatment, so billing teams avoid costly surprises later.

Automated checks inside Salesforce replace repetitive tasks, giving staff more time for patient support instead of chasing payer information.
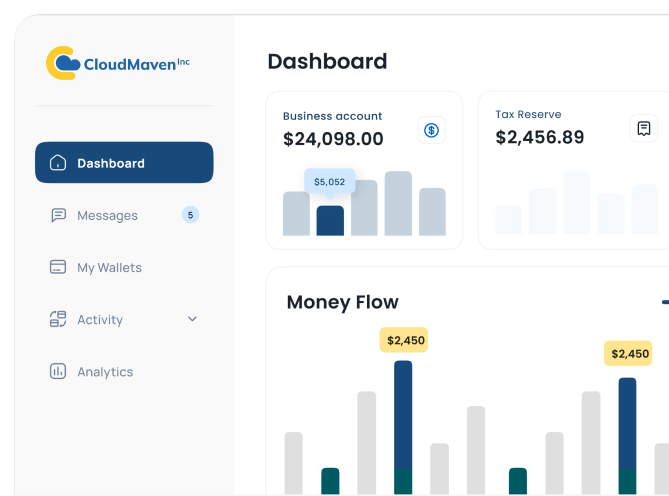
Why Healthcare Teams Prefer Our Medical Insurance Verification
With instant checks and fewer rejected claims, practices see real cost savings. Staff spend less time fixing errors and more time supporting patients.
You can see coverage for over 187 procedure types, helping teams spot gaps early and prevent billing issues before they ever reach the payer.
Built-in analytics help you catch patterns, track verification results, and adjust workflows. You get clearer visibility across departments without extra tools.

Once approved by the payer, you can verify eligibility for Medicare and Medicaid patients directly in Salesforce, keeping every visit cleaner and more predictable.
Accurate verification up front means fewer denials. Teams finally get relief from back-and-forth corrections that slow down reimbursement.
Instant answers free up your front desk and billing teams. No endless phone calls or portal logins; just quick, reliable information right in Salesforce.
With instant checks and fewer rejected claims, practices see real cost savings. Staff spend less time fixing errors and more time supporting patients.
Once approved by the payer, you can verify eligibility for Medicare and Medicaid patients directly in Salesforce, keeping every visit cleaner and more predictable.
You can see coverage for over 187 procedure types, helping teams spot gaps early and prevent billing issues before they ever reach the payer.
Accurate verification up front means fewer denials. Teams finally get relief from back-and-forth corrections that slow down reimbursement.
Built-in analytics help you catch patterns, track verification results, and adjust workflows. You get clearer visibility across departments without extra tools.
Instant answers free up your front desk and billing teams. No endless phone calls or portal logins; just quick, reliable information right in Salesforce.

Frequently Asked Questions
How does this app verify a patient’s coverage inside Salesforce?
Our Medical Insurance Verification app checks coverage in real time by pulling data directly from your connected payers. It confirms active insurance, benefits and out-of-pocket details instantly. This gives you fast and accurate patient coverage verification Salesforce results without calling payers or logging into multiple portals. Everything shows up clearly on the patient’s record so your staff can make confident decisions right away.
Can it validate insurance policies before treatment begins?
Yes, and it makes the whole process easier. Here’s what it checks:
- Whether the policy is active
- What benefits the patient has
- Any limits or exclusions you should know about
This built-in Insurance policy validation Salesforce workflow helps providers catch issues early and avoid costly billing delays.
Does it support Medicare, Medicaid and commercial payers?
Yes, Medical Insurance Verification connects to more than 950 payers, including major commercial carriers, Medicare and Medicaid. With this wide network, you can manage Medical insurance Salesforce tasks for nearly every patient who walks in. Most practices see fewer denials because coverage gaps are spotted before the visit even starts.
Will staff need extra training to use Medical Insurance Verification?
Not really. It works directly inside the Salesforce pages your team already uses, so they learn it quickly. Benefits for staff include:
- Simple clicks instead of long phone calls
- Coverage details shown in one place
- Fewer manual updates to patient records
This makes everyday Patient coverage verification Salesforce tasks much easier for busy front-desk and billing teams.
How does it help reduce claim denials and billing mistakes?
Most denials happen because coverage wasn’t verified properly. Our Medical Insurance Verification app fixes that by giving you accurate, real-time information before the claim is ever sent. It checks benefits, copays, coinsurance and required authorizations ahead of time. With stronger Insurance policy validation Salesforce processes in place, clinics see cleaner claims, faster payments and fewer write-offs.
Learn. Build. Grow.
.png)
December 13, 2023










.png)
.png)