cmHealth brings everything healthcare teams need including eligibility verification, intake, secure messaging, authorizations, and payments into one connected Salesforce experience. It reduces denials, speeds up approvals, and helps staff deliver faster, clearer, HIPAA-safe care without jumping between systems.

The Value Behind Connected Care
Real-time eligibility checks, automated authorizations, and integrated payments shorten claims cycles and improve cash flow across every line of service.
Upfront verification and accurate data capture reduce eligibility-related denials, prevent day-of-service surprises, and eliminate costly rework.
Eligibility, intake, communication, documents, and billing all run inside Salesforce, removing silos and creating a smoother experience for both patients and staff.
The Technology Behind Better Care
Automate medical insurance eligibility and verification with 900+ payers in Salesforce.
Generate, merge, split, digitally sign, and vault documents securely.
Automate and manage SMS, MMS, and fax communication.
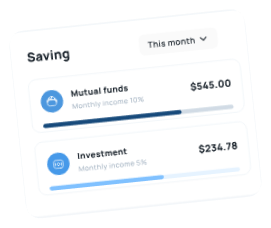
Robust payment solution to manage credit/debit cards, and ACH payments on Salesforce.
Benefits That Make Patient Care Smarter
Automated eligibility checks and streamlined intake reduce delays and keep claims moving without manual effort.
Encrypted email, SMS, fax, and eSign keep every patient interaction secure and fully compliant.
Real-time verification and integrated workflows prevent errors, missing details, and costly rework.
Connected communication channels improve clarity, reduce no-shows, and enhance the patient experience throughout care.
Coverage checks, forms, and authorizations run together in Salesforce, eliminating fragmented tools and extra steps.
Automation removes repetitive verification and intake tasks, freeing staff to focus on patient needs.
Frequently Asked Questions
How can I verify patient eligibility and benefits directly inside Salesforce?
Many healthcare teams connect Salesforce to real-time eligibility services so staff can confirm active coverage, benefits, copays, and referral requirements without jumping between portals. This reduces day-of-service surprises and helps prevent eligibility-related claim denials.
Can Salesforce help reduce insurance denials caused by incorrect coverage information?
Yes. When eligibility and benefits checks run before appointments, staff catch inactive plans, missing referrals, or outdated patient data early. This leads to fewer denials, less rework, and faster approvals from payers.
What does real-time medical insurance verification look like in Salesforce?
It typically works like this:
- Patient or member data is sent automatically to the payer
- Coverage details return within seconds
- Copays, deductibles, and limitations appear on the Salesforce record
- Everything is logged for compliance
This keeps intake and billing workflows moving without manual follow-up.
How do healthcare organizations manage referrals and authorizations in Salesforce?
Many clinics and health systems use integrated document generation and e-signature tools to create referrals, capture signatures, and store authorizations all within Salesforce. When eligibility and authorizations flow together, approvals happen faster and billing becomes more predictable.
Is insurance verification in Salesforce HIPAA-compliant?
It can be, as long as the system uses encrypted communication, secure messaging (email, SMS, fax), and tamper-evident records. Healthcare organizations often choose Salesforce-native tools so all eligibility checks, documents, and communications stay fully logged and HIPAA-safe.
Testimonials
Hear From Our Happy Customers